Maintaining vaginal health through regular gynecologic exams and Pap smears is the ideal way to do this, however you may also wish to conduct self-exams to become acquainted with what the vulva looks like as well as experience its normal tingle and scent.
Avoid using harsh cleansers and douching in the vaginal area as these may wreak havoc with its delicate pH balance and lead to yeast infections.
Diet
Your diet plays a key role in vaginal health, particularly with regard to its microbiome and pH levels. A diet rich in whole and minimally processed foods will promote overall wellness while helping your vaginal ecosystem remain at an ideal pH level to reduce infections while increasing lubrication and prevent infections.
Foods rich in Vitamin C such as citrus fruits, red, green, and yellow bell peppers (bell peppers are particularly high), strawberries are excellent ways to increase immune system functionality, fight infection effectively, and lower your risk of yeast infections. A low glycemic index diet also plays an integral part in decreasing this risk by helping keep blood sugar stable – all the better to combat infection!
An effective vaginal health regimen also relies on keeping yourself hydrated – another key aspect of vaginal health. Supplementing your diet with probiotics and omega-3 fatty acids may also help maintain an ideal balance of bacteria within your vagina, which will reduce odor and prevent inflammation. Fermented foods like yogurt and kombucha provide great sources of probiotics; also look out for prebiotics found in certain vegetables and herbs as sources. Ultimately, keeping yourself well hydrated is the cornerstone of vaginal health!
Exercise
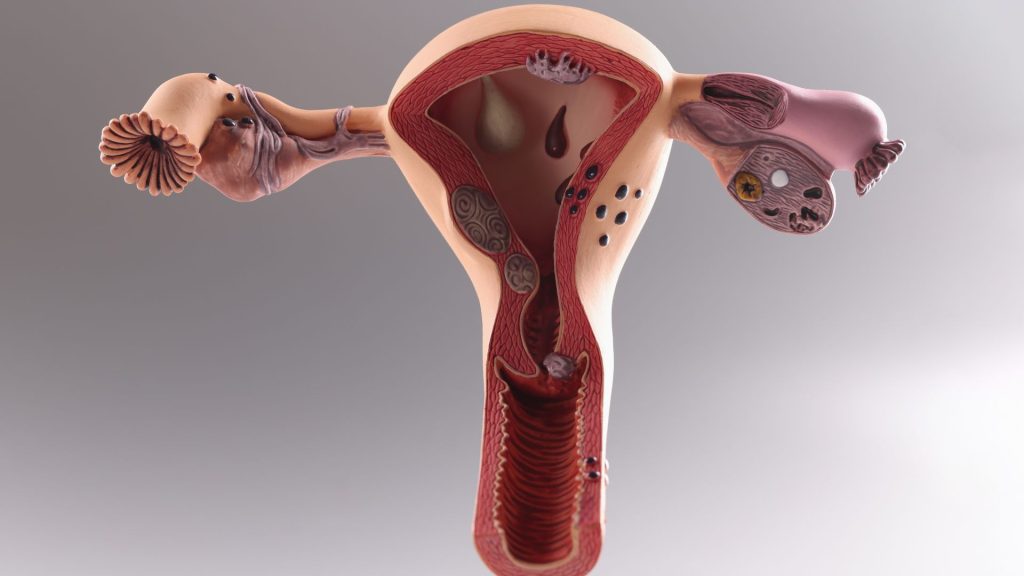
Exercise is essential to vaginal health, and engaging in 30 minutes of moderate physical activity four times each week for 30 minutes at least is recommended to maintain strong blood vessels and avoid conditions like prolapsed vulva (when the pelvic floor muscles weaken, and your bladder, uterus or bowel protrude into your vagina). Prolapsed Vulva is particularly prevalent among older women and can cause pain during urination or sexual activity – so Kegel exercises may be an easy solution that could prevent future incidents like prolapsed Vulva from ever happening again! Kegel exercises are portable exercises you can easily do anywhere while strengthening pelvic floor muscle strength – making Kegel exercises the ideal way to strengthen them and can prevent prolapsed Vulva from ever happening again!
As soon as you finish exercising, shower to remove sweat and dampness to ensure a pleasant workout experience. Excess sweat can provide the ideal environment for yeast and harmful bacteria to grow and cause irritation or infection if left on, so to protect yourself wear breathable cotton underwear and shower immediately afterwards. Using weighted vaginal cones (weighing roughly the same as a tampon) during Kegel exercises is another effective strategy.
Hygiene
The vulva (external part of the genitals) contains pubic mound, inner and outer labia, clitoris, and urethra, as well as its own special mix of bacteria that aids in maintaining an ideal pH balance that’s essential to vaginal health.
An optimally healthy vagina emits only a faint natural odor; however, an imbalance in this complex ecosystem may result in yeast infections, Bacterial Vaginosis or urinary tract infections.
To avoid such issues, daily gentle cleansing is key to staying healthy and preventing issues from arising. Avoid harsh soaps and instead opt for natural, fragrance-free over-the-counter wellness products designed specifically for the vulva.
Sexual Health
An ideal vagina is home to an equilibrium of different kinds of bacteria, with an acidic pH level to discourage bad bacteria from overgrowing quickly. When this balance shifts unexpectedly, however, problems such as bacterial vaginosis (BV), yeast infections or trichomoniasis may ensue.
These issues may cause itching, burning, swelling and discharge – it’s essential that an accurate diagnosis be obtained so the appropriate treatments can be implemented.
Sexually transmitted infections that impact the vulva such as chlamydia, gonorrhea, herpes and genital warts may also contribute to painful sex experiences.
Other causes of sexual discomfort can include psychological factors like low levels of arousal or fear of negative consequences from sexual contact; relationship dynamics like mistrust and emotional detachment; as well as hormonal fluctuations due to decreased estrogen production before menopause or breastfeeding (which may be mitigated through medications and other means). These issues can often be managed using medication and other modalities.